Severe, end-stage corneal blindness represents one of the most complex challenges in ophthalmology. These are patients for whom conventional corneal transplantation is unlikely to succeed or simply not possible — due to severe ocular surface disease, chronic dry eye, or multiple graft failures. In such cases, restoring vision is no longer a matter of replacing damaged tissue alone, but of navigating extreme anatomical, surgical, and clinical constraints.
One of the few viable solutions for these patients is the Osteo-odonto Keratoprosthesis (OOKP), commonly known as the “tooth-in-eye” procedure. While clinically effective, OOKP is an exceptionally complex, two-stage surgery. It involves harvesting a patient’s tooth and surrounding bone, months of tissue integration, and the coordination of multidisciplinary surgical teams. The procedure is costly, resource-intensive, and places a significant physical and psychological burden on patients.
It is within this highly specialised and demanding clinical context that a team of Singapore-based researchers is introducing a new approach: a 3D-printed keratoprosthesis (KPro) designed to replace the tooth-derived “skirt” used in OOKP with a precisely engineered implant. By leveraging additive manufacturing, the team aims to reduce procedural complexity, improve reproducibility, and open new possibilities for treating severe corneal blindness.

3D printed keratoprosthesis (KPro), photo credit: Temasek Polytechnic
The Challenge: Addressing Clinical and Systemic Constraints
Globally, an estimated 5–6 million people are bilaterally blind or severely visually impaired due to corneal opacity, with many more affected unilaterally. Although eye banking has expanded over the years, access to corneal transplantation remains uneven. There is approximately one donated cornea for every 70 patients in need, and more than half of the world’s population — particularly in low-resource settings — has limited or no access to transplantation services.
While donor shortages are a significant issue, keratoprostheses play a distinct clinical role. They are especially critical for a smaller but highly complex group of patients for whom standard corneal grafts repeatedly fail or are contraindicated altogether.
In these cases, OOKP remains one of the few viable solutions. However, the procedure requires harvesting a tooth, performing complex multi-stage surgery, and manually bonding a transparent, lightweight, and rigid thermoplastic optical cylinder to living dentine using acrylic resin — a process associated with technical challenges and long-term stability concerns.
This combination of surgical complexity, reliance on biological structures, and limited reproducibility has severely constrained the accessibility of OOKP in real-world clinical practice.
“OOKP has a proven track record over 60 years, but the procedure is labour intensive, costly, and requires multiple teams of surgeons both for tooth harvesting, ocular surgery, and follow-up. It also depends on biological tissue, which can have variable properties, and cannot be performed in many patients due to a lack of specialised teams that many healthcare systems simply do not have access to, or in edentulous patients. As a result, very few of the patients who could benefit from the OOKP are ever able to receive it. An all-in-one 3D-printed KPro can solve these problems,” says Professor Jodhbir Mehta, Executive Director, Singapore Eye Research Institute (SERI) and Clinical Advisor to the project.
The Breakthrough: A 3D Printed Window to the World
To address these challenges, researchers at the SERI and Temasek Polytechnic (TP) have developed a 3D printed KPro prototype that replicates the structure and optical clarity of a natural cornea, replacing the tooth-derived component with a Ti6Al4V (titanium alloy) skirt.
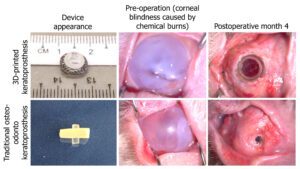
3D KPro (top) versus OOKP (bottom), photo credit: TP & SERI
Funded by the National Additive Manufacturing Innovation Cluster (NAMIC), the team applied advanced biocompatible materials and precision 3D printing to redesign the KPro architecture. The result is an optical cylinder with a built-in mechanical locking mechanism that can be assembled in less than a minute, with a wider field of view as compared to the traditional OOKP.
This innovation has the potential to significantly simplify the surgical workflow, reduce costs, and ease the logistical and emotional burden often experienced by patients.
Specifically, the 3D-printed KPro addresses key limitations of existing approaches by:
- Eliminating reliance on donor corneal tissue.
- Replacing the tooth-derived skirt with a reproducibly manufactured Ti6Al4V component.
- Introducing a mechanical locking interface, removing the need to manually glue the optical cylinder to a biological lamina — potentially improving assembly reliability and long-term stability.
“For implants where geometric intricacy and dimensional accuracy are critical, and inherently low production volumes, AM provides a production approach that aligns naturally with clinical needs,” says Dr Edgar Tan, co-principal investigator of the project. “Instead of one-size-fits-all, we can now shape the implant to follow the corneal curvature and embed channel structures into the skirt to enhance tissue anchorage, nutrient flow, and vascular support around the device.”
The materials are engineered for optical transparency, mechanical strength, and biocompatibility, ensuring stability within the eye while reducing the risk of rejection. Early laboratory and preclinical testing have demonstrated promising results in optical performance, tissue compatibility, and integration.
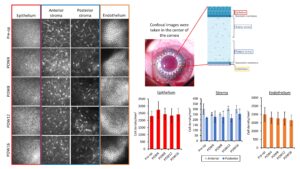
In vivo safety test images and results. Photo credits: TP & SERI
The Benefits: Affordable, Scalable, and Streamlined
The potential impact of this technology extends well beyond the laboratory. A 3D printed KPro could make sight restoration:
More Affordable
A simplified, single-stage procedure could lower overall treatment costs by up to 40%, making KPro-based solutions more accessible to hospitals that lack maxillofacial support, eye bank infrastructure, or the resources to run complex staged OOKP programmes.
More Scalable
Digital design and additive manufacturing enable consistent production of intricate skirt architectures and locking interfaces that are difficult to machine or mould. This supports greater standardisation, improved quality control, and smoother pathways toward wider clinical deployment.
More Streamlined
The KPro can be pre-assembled and sterilised, allowing ophthalmic surgeons to focus solely on implantation. With no multi-stage surgery required, procedures can be completed in a single session with significantly shorter operating times.
“Design and precision through additive manufacturing opens up a whole new dimension on implant technology,” says principal investigator, Mr Lee Khim Yong.
For healthcare systems, this translates into greater surgical efficiency and expanded treatment capacity. For industry, it represents a compelling opportunity to shape the next generation of ophthalmic and biomedical implant technologies.
From Lab to Market: A Call for Collaboration
The research team is now progressing towards preclinical testing and scalability studies, key steps before regulatory approval and clinical trials. To accelerate commercialisation, they are seeking industry partners, including medical device manufacturers, ophthalmic specialists, and medtech investors.

Photo of the research team from left to right: Mr Lee Khim Yong, Dr Edgar Tan, Dr Andri Kartasasmita Riau
“Our goal is to see this technology benefit patients worldwide,” says Dr Andri Kartasasmita Riau, who leads the project’s clinical design and translational strategy at SERI. “We welcome partners who share our vision, both literally and figuratively, to help us bring this breakthrough from the lab to the clinic, by co-developing the regulatory pathway, scaling up manufacturing, and exploring market entry in regions where current options are too complex, costly, or simply unavailable.”
Beyond the Eye: A Glimpse into the Future of Biofabrication
This project highlights Singapore’s rising leadership in biofabrication and advanced manufacturing for healthcare. The principles behind the 3D printed KPro: precision layering, biocompatible materials, and digital design, also underpin progress in artificial tissues, bone scaffolds, and organ-on-chip systems.
As additive manufacturing continues to merge with biotechnology, new possibilities are emerging for patient-specific medical devices and regenerative therapies.
What once sounded like science fiction — restoring sight with a 3D printed implant, is now approaching reality. With every breakthrough, researchers are not only redefining how we treat blindness, but also how we manufacture hope.

